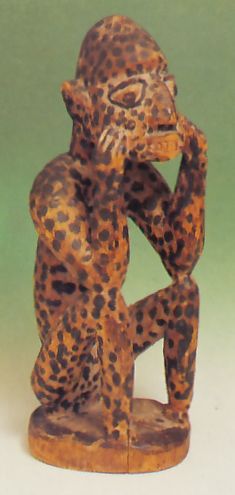
Yoruba Smallpox Spirit (Nigeria)
Around the world spirits have routinely been held to be the cause or cure (or both) of epidemic diseases.
|
Go to site main page, student resources page. |
Content Created: 2008-08-15. File last modified: |

Like other animals, humans have always shared their world with myriad microorganisms, both external and internal. From intestinal flora and parasitic worms or insect larvae to bacteria and viruses, each of us is host to a whole zoo of nano-life, some of which supports our existence, but some of which makes us sick or, in some cases, kills us.
Note 1 The less common (and unnecessary) term “pandemic” refers to an epidemic affecting, in theory, all people (after Greek pan- “all”). Since demos refers to people, for animals, the (also unnecessary) terms “epizoötic” and “panzoötic” are considered preferable by some people. A similar (unnecessary) distinction is made by some people between “endemic” (“found throughout a human population”) and “enzoötic.” (For plants, the term “epidemic” is normal for everything.)
This is unsurprising to us today, but until the invention of the microscope, the “life” of disease agents was largely unknown. Although some treatments were known to be effective, the reasons were obscure. The term “epidemic” refers to a rapidly spreading contagious disease affecting a great many people at the same time (from Greek epi- “among” and demos, “human population”). [Note 1]
This essay provides a quick overview of four major diseases responsible for devastating epidemics over and over throughout history: smallpox, flu, plague, and cholera. This is followed by a brief discussion of epidemic disease and the transition from foraging to farming. The essay closes with three brief case studies of human cultural responses to epidemics: a smallpox catastrophe in the northern Great Plains of North America, an epidemic (possibly smallpox or measles) described by the ancient Greek historian Thucydides and a XXth-century epidemic (cholera) witnessed by the Chinese ethnographer, Francis Hsu.
Smallpox (Variola major) is a viral disease spread by airborne spores. It is highly contagious. In Afro-Eurasian and modern populations, untreated smallpox results in death within ten days to a month of first symptoms in about a third of the cases. Death rates were considerably higher for indigenous populations when smallpox first arrived from Europe with Spanish explorers in the Americas.
Note 2 Usage note: The individual pustules are called “pocks,” not “pox.” In contrast, the word “pox” refers to any disease which produces pocks. In earlier English, “pox” could also refer more broadly to any calamity, as in “A pox upon thee!”
For the first week or two after infection, the victim shows no outward signs of infection. Suddenly, for three or four days —in what is called the “prodromal” or initial symptoms stage— the victim suffers bad headaches, high fever, chills, backache, vomiting, and often delirium. This is soon followed by a rash of red spots that become puss-filled “pocks” both on the skin and inside the mouth and throat, but especially on the hands and feet and the face. [Note 2] When they burst, the pocks become foul-smelling sores, eventually producing obtrusive scars (pock marks) among survivors, who may also be left blind. However survivors, although scarred, are left with a life-long immunity to the disease.
Building on this immunity doctors developed the technique of vaccinating uninfected people with dead smallpox spores, causing the body to develop the necessary antibodies, and conveying the immunity without the disease itself. This public health measure was already available in Europe and America by the late 1700s. The last known case in the United States was in 1949. By 1980, in an unprecedented triumph of international cooperation, smallpox had been entirely eradicated throughout the world except for experimental collections maintained at State Research Center of Virology and Biotechnology in Russia and at the Center for Disease Control and Prevention in the United States. There was some international pressure to destroy these stocks and thus end smallpox forever, but they were retained so as to maintain a capacity to develop treatments in case terrorists or rogue states should gain access to a smallpox source that might have been overlooked, or in case some other pox virus mutated into a similar form. Despite a small danger of the virus stocks getting “out” and killing millions once again, smallpox appears to have been conquered.
Smallpox was historically one of the worst kinds of epidemics because of its high mortality rate and ease of contagion. It probably first emerged in India or Egypt and may have been carried to Europe in Roman times, spreading to other areas during the European age of exploration. Smallpox is believed to have killed more people than any other infection in human history, including the Black Death of the Middle Ages. In the XXth century it is estimated to have killed between 300 and 500 million people, or possibly more. In 1967 alone there were about 15 million new cases and about 2 million deaths.
One reason why smallpox was such a scourge was that the virus could remain alive and infectious for up to a year and a half in more or less room-temperature clothing which had once been in contact with the scabs or bodily fluids of a victim. Thus smallpox was easily spread by accident (or at times perhaps deliberately) through infected blankets or garments, and could easily be spread to individuals or populations who had no direct contact with earlier victims.
Influenza is an extremely contagious disease caused by any of several related viruses. It produces fever, muscle aches, vomiting or diarrhea, and severe inflammation of the mucus membranes of the upper respiratory tract, producing a stuffy and/or runny nose. Many flu viruses are able to survive outside of their animal carriers for up to eight hours, and hence flu can be spread by infected objects.
Depending upon the year, between a quarter of a million and a million deaths a year can be attributed to influenza (usually about 35,000 or so in the United States). The viruses involved reproduce rapidly with high mutation rates, so they can mutate beyond the reach of available vaccines and established immunities, producing periodic widespread outbreaks. It appears that a general flu pandemic, caused by sufficient mutation that people’s established immunities no longer work, occurs every two or three decades.
Bird Flu (Avian Influenza, H5N1 Flu). Several types of flu seem to be hosted by birds, and researchers suspect that human flu types may have originated with the mutation of widespread avian strains that might not always have been immediately fatal to their original feathered hosts. So far transmission of today’s “bird flu” (technically, “Influenza A virus subtype H5N1”) is between birds and, occasionally, to a human. It is being carefully monitored because public health experts fear that a variant could develop that is easily spread between people. Should that occur, millions of human deaths could be caused before the epidemic ran its course.
Swine Flu (H1N1 Flu). H1N1 swine flu became a serious threat in 2009. This swine flu does not infect hogs, and almost certainly did not begin as a disease of swine. According to the Centers for Disease Control and Prevention website (5/5/2009):
… laboratory testing showed that many of the genes in this new virus were very similar to influenza viruses that normally occur in pigs in North America. But … this new virus is very different from what normally circulates in North American pigs. It has two genes from flu viruses that normally circulate in pigs in Europe and Asia and avian genes and human genes. Scientists call this a ‘quadruple reassortant’ virus.”
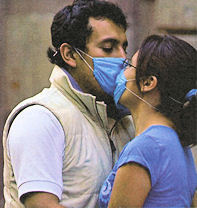
Today’s swine flu is almost exclusively a human disease, spreading from one human to another, and remarkable for being even more contagious than most other kinds of flu. It can be contracted from touching objects contaminated by coughing, sneezing, or touching by infected people, but it is mostly contracted directly from other people, just as seasonal flu varieties are. People can be carriers for a day or so before they show symptoms, and for up to a week after they get sick. It became an object of great concern to public health authorities in the spring of 2009, when cases rapidly spread from Mexico to Texas and California and then around the world, bringing several fatalities. (The global death toll was about 300,000.)
Spanish Flu. The most famous flu outbreak was the “Spanish Flu” of 1918-19, which is believed to have killed between 20 and possibly even 50 million people worldwide (about a half million in the United States). Some estimates are higher, as many as 100 million deaths worldwide and infection of perhaps a third of the world population. In Europe, it produced at least twice the casualty rate of the First World War.In India it wiped out about six percent of the entire population. (Despite the name “Spanish Flu,” it is now believed to have emerged first in Kansas, not Spain, and to have spread to Europe with American soldiers.) For unknown reasons, Spanish flu tended to target young, healthy adults, and this population accounted for about half of all the Spanish Flu deaths.
With progress in the study of genetics, it has been possible to see RNA signatures of Spanish flu in modern flu variants, including swine flu and bird flu, so arguably it is still with us.
Perhaps because the symptoms are so generic, there is little clear evidence for flu before the 1800s. Other, lesser flu epidemics since the Spanish Flu included the 1957-58 Asian Flu (70 thousand deaths in US), which affected 10 to 35 percent of the world’s population, and the 1968-69 Hong Kong Flu (which affected about 30 million Americans, although it caused “only” about 34 thousand deaths in US). Each of those epidemics caused about a million deaths globally. Fortunately, modern understanding of the flu virus and its many mutations is far deeper than ever before.
The word “plague” is often used as a generic term for an epidemic, or even a troublesome insect invasion. However it more exactly refers to infection by a specific and extremely contagious bacterium, Yersinia pestis (formerly called Pasteurella pestis), of which three different varieties have been responsible for plague epidemics in different parts of the world (Biraben 1977: 26). Infection leads to death in most infected individuals within about a week if untreated. It is said that more humans have died of plague than have ever died in war. The disease is now treated with antibiotics.

Bubonic Plague. Bubonic plague is a specific manifestation of plague. Symptoms of bubonic plague infection include: high fever, chills, painfully enlarged lymph nodes, especially in the groin, which turn black in the “black plague” form of the disease (Such swellings are called buboes —the origin of the term “bubonic”— and are also characteristic of some other diseases, such as syphilis.)
Bubonic plague swept Europe as the Black Death between 1347 and 1351 (lasting even longer in some areas), and it is estimated to have killed as much as three quarters of the population of the most heavily affected areas over the course of two decades. It probably killed about a third of the population of Europe as a whole.
Smaller plague outbreaks continued in Europe until the early XVIIIth century. (The photo shows a waxwork of a XIVth-century plague doctor wearing protective clothing, including a waxed cape and a face mask stuffed with strong-smelling herbs, measures believed to help protect him from infection. The stick was his protection against patients who tried to get too close.)
The Life of a Plague Bacillus. The plague bacillus finds a favored breeding ground in the blood of rats, but rats are also hosts for fleas (most notoriously Xenopsylla cheopis), which live on their blood, from which the fleas ingest the bacillus. The bacillus clogs the flea’s proventriculus, a kind of pouch on the esophagus of the flee that is part of its normal food tract. This congestion causes the hungry flea to seek additional food, often from the blood of another rat, into whose bloodstream it regurgitates part of its previous intake of food, infecting the new rat.

The fleas most associated with the plague much prefer rats to humans, and it is unclear how often they transmit the plague bacillus to humans.
One should emphasize that different species of flea have a marked specificity for a given host, except temporarily in the very rare cases where they cannot find their normal host. The cat flea lives only on the cat, the dog flea on the dog and so on. There are only a few exceptions … . In practice, Coratophylus fasciatus lives indifferently on wild and domestic rats and so ensures the transmission of plague from one to the other, and Xenopsylla cheopis, which lives on domestic rats can, in the absence of rats, bite man. (It is the same with the mouse flea, Leptopyslla musculi, which cannot transmit plague from mouse to mouse but occasionally bites domestic rats, although never man. Sometimes however, as in Madagascar, mice have Xenopsylla cheopis as parasites.) It is this latter flea [Xenopsylla cheopis] which is responsible for passing plague from rat to man, and for a long time it was thought that it alone was responsible for all epidemics, both because it plays a role in modern epidemics, and because the human flea, Pulex irritans, has no proventriculus. But Pulex irritans, which lives only on man, readily transmit the disease, and its importance depends on the number of humans infected. (Biraben 1977: 29-30)
Note 3 The bacillus can survive only briefly when exposed to light and air or varying temperature, but can survive for “months and sometimes even years if kept in the dark and at a constant temperature, as in a sealed test tube in a laboratory, or underground, particularly in the microclimate of rodents’ burrows” (Biraben 1977: 26).
Thus, although bubonic plague sometimes can be transmitted without rats —indeed the bacillus can be transmitted from a recently infected inanimate object [Note 3] to a human sore or cut— historically it has required a population of rats for its spread as an epidemic. (That is not true of the pneumonic form, as we shall see.) Rats are clearly implicated in the devastating plagues known to European history. [Note 4]
Note 4 Black rats or house rats, Rattus rattus, seem especially implicated; brown rats, Rattus norvegicus, commoner today, do not as readily host the bacillus. The understanding that plague was associated with fleas came earlier to Europe than the details of its connection to rats,. In 1665 the Lord Mayor of London ordered the widespread destruction of cats and dogs in hope of controlling a plague outbreak, and made matters worse because the action removed the predators that normally controlled the rat population.
Pneumonic Plague. Bubonic plague is usually not contagious among humans. However, once the virus enters human lungs, it produces pneumonic plague, involving respiratory failure and collapse of the circulatory system. While the patient briefly remains alive, pneumonic plague can easily be transmitted between people through droplets expelled through sneezing or coughing and then inhaled by other people directly into their lungs. This makes pneumonic plague extremely contagious for humans, even while bubonic plague is not.
Pneumonic plague can pass with ease between people, so once the plague has been established when a rat is bitten by an infected flea and in turn bites a human, a human pneumonic plague epidemic can be produced and sustained with no further involvement by rats or fleas.
Note 5 The Great Plague of London of 1665-1666 is believed to have killed about 17% of the population of London and is known to history through the diaries of Samuel Pepys, who lived through it, and an account by writer Daniel Defoe, whose uncle did. Probably important to the end of the plague was the Great Fire that broke out in 1666 and destroyed much of the rat population. The Great Plague did not spread to most of the British countryside, due in part to vigorous quarantine efforts. Eyam, where the percentage death toll was much higher (although probably nothing like the three quarters sometimes mentioned), was therefore unusual (and scary) (Clifford 2003: 20-23). Eyam became an especially significant footnote in history because extremely quick, united, and enlightened local action, largely free of political grandstanding, produced a self-quarantine, confining the deadly outbreak to Eyam and sparing surrounding villages.
Fleas sometimes reside for a time in clothing or bedding, as well as laying eggs there, and thus plague can sometimes spread with trade in cloth, which carries fleas to a new area, where they affect a new rat population when released from the cloth at its destination. The well-documented plague at the village of Eyam in Britain (1665-1666) was believed to have been transmitted from plague-stricken London by means of an old coat purchased by a local tailor who wished to copy the style. A flea in the coat apparently infected a rat in the tailor’s shop. Two weeks later the tailor was dead and within another fortnight others were dying throughout the village. [Note 5]
Nowadays, there are between 150 and 200 deaths world-wide attributable to plague. In the United States, where plague is most common in the southwest, there are usually under fifteen cases a year, although there was a slight increase after an epidemic among prairie dogs in northern Arizona in 2007. Worldwide, about 14% percent of modern human plague cases are fatal.
Cholera [KAHL-er-ah] is a disease of the small intestine caused by the bacterium Vibrio cholerae. It tends to be especially severe in older children and in adults. The characteristic symptoms are severe diarrhea, usually accompanied by vomiting, resulting in severe dehydration (and desalination and depletion of electrolytes), producing severe thirst, painful muscle cramps, and eventually circulatory collapse. The most obvious treatment involves administering huge amounts of water, most of which, however, is vomited up or passed in diarrhea. In countries where cholera epidemics occur, a “cholera bed” is sometimes made, a kind of cot with a hole in the middle through which the almost continuous diarrhea can drain into a tub below rather than filling the bed itself (Werner 1977: 158).

Untreated, cholera is fatal about half of all cases, and death can come as soon as a few hours after the first symptoms appear, although death rates are very much lower when modern antibiotics are applied.
Cholera can be spread from infected people through the air, but is usually transmitted through infected drinking water. Simply boiling water before its use is one simple and ancient public health measure that can potentially reduce the impact of an outbreak, although of course it does nothing for those already infected. Since people in the past rarely knew why it worked, many doubted that it did.

The cholera bacterium thrives at a temperature of about 27°C (81°F), but does not survive well in temperatures below 15°C (59°F) or above 42°C (108°F). Outbreaks therefore tend to be confined to tropical regions or to near-tropical regions during warm periods, especially where there is great population density and contaminated water. A change of temperature for a time can end an epidemic.
In the early years of the XXIst century, worldwide about a quarter million people a year contracted cholera, and death rates averaged from one to four percent. But the numbers vary from year to year and region to region. For example, after the disastrous earthquake in the Caribbean nation of Haiti in 2010, apparently a sewage leak from an encampment of UN peacekeepers from Nepal polluted a local river in the Artibonite Valley, about 100 km north of the devastated capital of Port-au-Prince. The pollution carried a southern Asian strain of cholera into the local population. The sewage leak occurred in October of 2010. Despite the early and vigorous efforts of international health workers to avoid and later to stop the epidemic, by March of 2011, six months after the sewage spill, over 250,000 cholera cases had been identified, and nearly 5,000 people had died, or about 2% of those infected. A year later, in March of 2012, the infection rate had risen to half a million, and the death rate to about 7,000, about 1.5% of those infected. (The UN admitted responsibility only in 2016.)
In general, Upper Paleolithic foraging populations were healthier than Neolithic populations. The bodies that have come to us from archaeological sites of such foragers show injuries, sometimes fully or partially healed and sometimes fatal, and they occasionally show starvation or seasonal malnutrition. But for the most part foragers had a sufficiently diverse diet over the course of the year to keep them generally healthy.
Note 6 Environmental factors other than diet can influence the general health and disease susceptibility of a population, of course. In modern times, industrialization with its associated pollution and sedentary life style has been held responsible for rising levels of heart disease, diabetes, and especially cancer, although the mechanics are still unknown. (Cancer is not easily detected when all that remains is skeletal material, but in some cases we have better preserved bodies. Mummies from agriculturalists in Egypt and Peru and from foragers in Alaska show no cancer.)
In contrast, Neolithic diet became more and more dominated by the far smaller range of plants and animals being cultivated, despite some supplementation with foraged foods. A deficiency disease like beriberi or rickets, caused by a restricted range of foods, is far more likely to be evident among skeletons of early farmers than of terminal foragers. Study after study of the skeletons of early farmers shows shorter stature and shorter life expectancy than among foragers (Rudgley 1999:8.). It is reasonable to think of early farmers as a nutritionally weakened population, and we should therefore expect greater susceptibility to whatever diseases came along. [Note 6]
At least two additional factors also tended to contribute to poorer health among early farmers. One was the possibility of diseases spreading from domesticated animals to humans, especially in climates where they shared shelters. It is unusual for diseases to jump from one animal species to another, but it also not unknown. Leprosy, for example, appears to have derived from an ailment of the Asian water-buffalo. Malaria and HIV seem to have started among chimpanzees. Bird Flu has sometimes made the jump from birds to people. Ebola can be spread from people eating the meat of infected bats and chimpanzees, animals that are able to carry this disease. SARS and HIV appear to have jumped from animals to people as well. Milk is capable of spreading nearly thirty different diseases, including diphtheria.
Hunted animals could also bring disease, of course, as their meat was eaten and body parts handled. This danger would probably have been more widespread when they were exchanged in Neolithic markets than when they were consumed by small hunting bands, which brings us to the second factor.
The second factor was greater population density among agricultural societies, so that diseases could spread easily from person to person as they could not between small hunting bands. Disease was also spread due to the greater difficulty of keeping clean water supplies from being contaminated by waste materials as population density increased.
The renowned science writer Jared Diamond has argued that these factors —intimacy with domestic animals and population density— are the two main reasons why Eurasian diseases did not come to the Americas until the Spanish arrived. The small bands that lived in and eventually crossed Beringia (the Bering Strait) had no domestic animals and lived in small bands. Any truly serious disease might wipe out a band, but that would mean the band could not propagate the disease further. In addition, many of the major diseases that afflicted the New World populations after the Spanish arrived (for example, smallpox and measles) confer long-term or lifetime immunity to those who survive them. A population must be fairly large to keep such disease organisms alive, “fed,” and reproducing. The small bands traversing Beringia into the New World, were too small to “support” diseases that confer long-term immunity, so such disease organisms tended to disappear in those populations.
These two facts —few domestic animals and small group size— Diamond argues, provide the reason why European diseases had such devastating effects upon the peoples of the New World after the Spanish arrival, who had retained no immunity to them (Diamond 1992).
However another factor was probably the fact that Beringia was cold. Weather was usually below the temperature at which the bacillus or virus causing major disease outbreaks in Eurasia could be transmitted easily, creating a “cold filter” that prevented these disease organisms from surviving and spreading among subarctic populations slowly moving towards the Americas.
Click here for a brief essay on Beringia.
One rarely has a sufficient number of specimens to see an epidemic clearly in archaeological evidence. We have a few accounts of ancient and historical epidemics, although in early accounts it is sometimes quite difficult to be sure what the disease was from which so many are said to have died.
Note 7 The pestilence is sometimes called the “Antonine Plague” after the Roman royal house. But more often it is referred to as the “Plague of Galen.” Galen (129-199) was the most famous physician of Classical antiquity. The renowned healer did not die in the plague that bears his name because he fled Rome to his estate in the countryside, staying away as far as he could get from infected people.
For example, an epidemic struck the army of the Roman general Lucius Verus (130-169) in AD 165, when it was engaged in wars against various Germanic tribes during the reign of Emperor Marcus Aurelius. The situation became bad enough that Verus’ armies suspended the war from about 166 to 169. When they were healthy enough to resume fighting, they found whole towns abandoned, and the bodies of German soldiers who had expired with no wounds. The epidemic, which seems to have originated in Iraq, swept across the Roman Empire. The emperor himself wrote of caravans of wagons hauling bodies of victims from Roman cities. Historians have no idea how much of the imperial population died in this great disaster. Estimates range from about one percent to as high as half. It is unknown what the pathogen was. Both measles and smallpox are suspected. [Note 7]
A century and a half later, another epidemic, probably smallpox, struck the Egyptian city of Alexandria (part of the Roman Empire), probably killing about two thirds of its population.
We have already mentioned the devastation of the Black Death, the plague epidemic of the 1300s (which was followed by the Great Plague of the 1600s). In 1707, another epidemic, again probably smallpox, killed perhaps a third of the population of Iceland. And so on.
The point is that humans have co-evolved with countless viruses and bacteria. Diseases, individual and population-wide, minor and major, have been part of the human story from the beginning, but massive epidemics appear to have become even more important after the development of population densities based in farming and eventuating in cities. Ancient cities would be regarded as filthy and pestilence ridden even by the standards of the most inadequate modern refugee camps. Until very recently, every city was a public health catastrophe waiting to happen. Or happening.
Swine Flu (2009). As we saw earlier, swine are not really involved in the transmission of today’s Swine Flu, but the name led to some interesting “public health” efforts early in 2009. The Kabul zoo, home to the only pig in Afghanistan, placed the animal in solitary confinement to avoid having it stoned by mobs convinced that it was a disease agent. Because the epidemic seemed to start in Mexico, Chinese authorities quarantined all visiting Mexican nationals, including anybody merely changing planes, to avoid the spread of the disease to China. The Egyptian government took advantage of public concern as an opportunity to slaughter all of the country’s pigs, which nearly always belonged to Coptic Christians, whom the majority Muslims have held in suspicion for centuries, and who were widely believed not to have supported the winning party in the previous election. In Israel the government, at the suggestion of the chief rabbinate, declared that the official name in Hebrew would be “Mexican Flu,” so that pious Jews would not have to pronounce the polluting word “swine.”
None of these unrealistic responses (with the remotely possible exception of the Chinese quarantine) could have any effect upon the Swine Flu. But all of them were sponsored by XXIst-century governments in response to a potential global health emergency.
The Covid-19 Pandemic (2020-22). Humanity has long coexisted with various kinds of coronavirus, several of which produce what we call the “common cold” (more). One coronavirus, technically referred to as SARS-CoV-2 and genetically similar to several other viruses found in China, seems to have jumped from a bat to a pangolin, and then to a human at the end of 2019, probably in a central Chinese market illegally selling pangolins as food (evidence).
SARS-CoV-2 produces an astonishingly contagious and quite dangerous, flu-like disease called Covid-19, which became a world scourge beginning in the first months of 2020, precipitating well over a year of stay-at-home orders and the wearing of facial masks around the entire world.
Like all viruses SARS-CoV-2 mutates, and genetic studies suggest that not long after it was initially recognized as dangerous, a mutation took place somewhere in Eastern China (referred to as the 614G variant) that grew and spread faster. Although both variants spread around the world, it appears that 614G may have been responsible for a "second wave" of infections in some countries after it appeared that the initial infections were coming under control.
Late in 2020 and early in 2021, yet more contagious variants, identified by letters and numbers, arose in Britain (B.1.1.7), India (B.1.617), California (B.1.427, B.1.429), South Africa, Brazil, and elsewhere, and the variants more important for public discussion were named after letters of the Greek alphabet. Variation B.1.617.2, “Delta,” proved to be particularly contagious and subsequent “Omega” (in more than one variant) even more contagious, but less deadly. By April, 2022, known cases had passed 500 million worldwide. Most cases were unreported, however, because they were unrecognized, because testing facilities were unavailable, because governments feared embarrassment for poor policies, or, by 2022, because people who tested themselves but had only mild symptoms feared being subjected to burdensome quarantine restrictions. A World Health Organization study released in May of 2022 estimated that worldwide “excess deaths” attributable to the virus were probably about fifteen million by that time.
Compared with many previous epidemics, Covid-19 generally stimulated more scientific and more realistic official responses (as well as a certain amount of political opportunism and/or official denials). Nobody used it a pretext to kill pigs. But individual conspiracy theorists damaged public health efforts in their eagerness to create absurd perspectives.
Some religious leaders argued that Covid-19 was caused by gay pride parades or increasing acceptance of gay marriage (examples), and once vaccinations began in Iran, Ayatollah Abbas Tabrizian, long a critic of non-Iranian medicine, told his nearly 21,000 followers, “Don’t go near those who have had the COVID vaccine. They have become homosexuals.”

John Magufuli, president of Tanzania, recommended attending churches on the grounds that the virus, being satanic, “cannot survive in the body of Christ.” And the central Asian nation of Turkmenistan, in a fit of unrealistic denial, banned the word “coronavirus” from all state media or health brochures and began arresting people daring to wear protective face masks in public or to discuss the virus in public.
In the United States, religious objections were also raised against common public health measures taken to reduce the spread of the virus. For example, a major public health measure was the use of masks covering the nose and mouth to prevent microscopic “droplets” moving from one person to another. A frequent non-religious objection claimed that this abridged personal freedom. But in Lansing, Michigan, the Resurrection School opposed a state mandate for masks to reduce transmission in schools arguing that “… because God created us in His image, we are masking that image … [which] is disruptive to this element of the Catholic faith.” (The Week, 2020-08-06 p. 6) As the worst effects of the Covid-19 virus were gradually reduced through a massive vaccination campaign, rumors were spread that the vaccination itself was dangerous, and eventually that all vaccination was dangerous. By the time of Donald Trump’s second term as U.S. president, he found it politically advantageous to appoint an “anti-vaxxer” to head the Department of Health and Human Services, and a political campaign was begun to withdraw government funding from vaccine development and to stop requiring school vaccinations. Lower-level public health workers immediately predicted a resurgence of formerly serious diseases in the years ahead.
As in earlier epidemics, the rapid spread of Covid-19 provided ample opportunity for mountebank cures, ranging from for-fee prayers of guaranteed effectiveness to exotic "snake-oil" medicines (example).
In contrast to earlier epidemics, an enormous influx of public money into established pharmaceutical laboratories in many countries resulted in the fastest development and production of promising vaccines in medical history, and the probable suppression of it as a major public health threat by the end of 2022.
The Past. What happened in earlier times? We proceed now to three historical cases to see some of the ways in which epidemic disease affected earlier communities and the nature of their responses.
Because smallpox showed no symptoms during its incubation period, newly infected sailors were sometimes recruited with no one aware that they were carriers until they were already at sea. Smallpox was one of the most deadly diseases brought to the Americas with the first European explorers, and it is said that it, together with measles, cholora, and pneumonia, probably wiped out about half of the population of the Aztec empire and even larger proportions of many other populations throughout the Americas.
The population of the Caddo, who lived in Texas and along the lower Mississippi River, was cut down in successive epidemics from perhaps 200,000 to as few as 10,000. Half of the Pawnees died in the early 1830s. The Blackfoot, once lords of the northern Plains, were reduced by two thirds in the great smallpox epidemic of 1837, brought up the Missouri River by traders. (Powers 2015:8)
The 1837 epidemic provides a reasonably well documented example of what happened among the culturally similar Hidatsa and Mandan tribes of North Dakota. The Mandan had been struck by smallpox in the 1780s, and by the time they were contacted by Lewis and Clark in 1804, they had been reduced to only two villages. (Ibid.)
In 1837, the United States was in the throes of an enormous investment enthusiasm, building a speculative economic bubble that burst on May 10 of that year with a stock market crash and a run on the banks, causing their bankruptcy. This in turn caused (1) government regulatory paralysis as politicians blamed each other and debated what to do, and (2) a five year depression (called a “panic” in those days), widely blamed on newly elected President Van Buren because he was president.
Note 8 The following inset quotations are assembled from several different display signs designed to provide a concise overview for museum visitors at Fort Mandan. Original sources were not provided.
The North Dakota story begins with a fateful decision made by the captain of a vessel belonging to the American Fur Trading Company. The boat set out from St. Louis and proceeded up the Missouri River on a mission intended to procure a year’s supply of animal pelts through trade with the closely related Mandan and Hidatsa tribes, and, largely through them, with other tribes of the upper Great Plains. A display in the Fort Mandan visitors’ center in 2009 vividly described the situation this way: [Note 8]
On April 17, 1837, when the steamboat St. Peter’s left St. Louis, a deck hand was already infected with smallpox and didn’t know it. By the time the disease was diagnosed [sometime before April 29, when the St. Peter’s docked at Fort Leavenworth], everyone on the boat had been exposed.
An Indian agent on board urged the captain, Bernard Pratte, Jr., to remove the sick man from the boat at Leavenworth, but the captain refused. By the time the boat reached Council Bluffs, others on board were ill. Still, the St. Peter’s continued to move up the Missouri in spite of the fact that it was carrying the deadly disease.
The vessel would probably still have been on the river when word would have reached them of the stock market crash and the bank failure, and it would have been obvious both to the ship’s captain and to others that the pelts were critical to the future of the financially challenged company. Depending upon the exact timing, it is possible that this could have been a factor in the captain’s seemingly callous decision not to offload the sick crewman at Fort Leavenworth.
The U.S. government had appropriated funds to vaccinate all the tribes along the Missouri, but the program [met resistance and] was stopped before doctors reached the Mandans and Hidatsas. [About half of the Arikaras and many of the Sioux tribes had been immunized by 1832.]
One of the Indian agents on board, Joshua Pilcher, sent word upriver that Indians should be instructed to keep away from the boat as it ascended the river.
These precautions proved impossible to enforce in the press of activity that greeted the St. Peter’s when it landed at Fort Clark on June 18, 1837. Fort Clark agent Francis Chardon noted that the merchandise on board was offloaded and stowed in the fort. Ominously he wrote, “all hands a Frolicking.” Some of the frolickers were carrying the deadly virus.
The first Mandan death from smallpox was recorded in a diary entry by Chadron a little under a month later, on July 14, 1837: “A young Mandan died to day of the Small Pox — several others have caught it.”
… because the first reported Mandan death did not occur until 26 days later, the virus was probably not spread by direct contact. Some of the supplies, however, may have been contaminated and later caused the infection. Another possibility is that the virus was spread from the boat on the return stop.

Among those who died in July of 1837 was a remarkable Mandan war leader named Mató Tópe (“Four Bears”), known today primarily because he was a picturesque subject for several white painters, but also for his own sketches of the long and sad history of Mandan warfare with the Cheyenne. He is said to have offered the following perspective as he lay dying:
My friends one and all, listen to what I have to say. Ever since I can remember, I have loved the Whites. … But today, I do pronounce them to be a set of black hearted dogs. They have deceived me, [they whom] I always considered as brothers. … I do not fear death, my friends. You know it. But [I fear] to die with my face rotten, [so] that even the wolves will shrink with horror at seeing me and say to themselves, “that is Four Bears, the Friend of the Whites.”…
(edited from Powers 2015: 8)
By that fall there were only 138 Mandan left (ibid.), and by the time winter set in, about 1,500 Mandan had died, and fewer than 100 were still alive: about a 90% death rate (Thybony 2007: 14).
The Hidatsa and Mandan were sitting targets for smallpox. They had no prior immunity, and they lived in heated earth lodges constructed close to each other, each sheltering a broadly extended family, and maintaining a temperature which, by sad coincidence, was nearly perfect for the smallpox virus. The Hidatsa and Mandan were especially badly hit. It is said that death rates of between a quarter and half affected the Blackfoot, Crow, Pawnee, and Assinoboines tribes (in addition to many deaths in preceding decades). In the Upper Missouri region as a whole, about 17,000 people are said to have died, estimated to be about a quarter of the population.
Among the Mandan and Hidatsa, the catastrophe resulted in an increased need for cooperation in defending their diminished communities against their shared enemy, the Sioux. A fascinating, if surprisingly matter-of-fact, account of this situation comes from the autobiography of a woman named Waheenee (“Buffalo-Bird Woman”), who was born two years later, in 1839, and who dictated her story in Hidatsa to ethnographer Gilbert L. Wilson between 1908 and 1918.
“The Mandans lived in two of the villages, the Hidatsas in three,” [Grandmother] said. …
“We had corn aplenty and buffalo meat to eat in the Five Villages, and there were old people and little children in every lodge. Then smallpox came. More than half of my [Hidatsa] tribe died in the smallpox winter. Of the Mandans only a few families were left alive. All of the old people and little children died.”
… Enemies gave our tribes much trouble after the smallpox year, my grandmother said. Bands of Sioux waylaid hunting parties or came prowling around our villages to steal horses. Our chiefs, Mandan and Hidatsa, held a council and decided to remove farther up the Missouri.
“We will build a new village,” they agreed, “and dwell together as one tribe.” (Waheenee 1921: 10)
Note 9 Their combined village was named Like-a-Fishhook. It was later flooded by the Garrison Dam and is now at the bottom of a reservoir, ironically named Lake Sakakawea, commemorating a Shoshone woman who was a Hidatsa only by virtue of abduction.
The Mandan and Hidatsa (and the Arikaras) had been tribes of semi-transhumant “village Indians,” dwelling, farming, and hunting bison on the banks of the Missouri for centuries, and had been part of the thriving fur trade, conducted largely with French fur traders after 1738, when the Mandan were first contacted by fur trader Pierre Gaultier de Varennes de La Vérendrye and a group of (unwelcome) Assiniboin tribesmen who had been his earlier fur trading partners (Meyer 1977: 18-19). The social effect of the smallpox catastrophe was a realignment of the system of inter-tribal relations, including the unification of the two tribes, effectively agreeing to merge their cultural identities, as they made common cause in the face of whatever the future might hold for them. [Note 9]
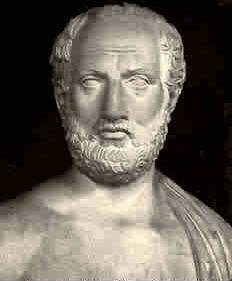
Thucydides was an ancient Greek historian, known for his History of the Peloponnesian War. In one passage he described how people from the countryside around Athens had taken refuge within the city walls, increasing its population density, and hence its ability to sustain an epidemic. He then describes the epidemic that did in fact strike in 430 or 431 BC. Thucydides tells us that the epidemic seemed to have started in Ethiopia and been transmitted down the Nile and along the African coast of the Mediterranean, where it was carried to Greece by trading ships.
Symptoms included high fever and severe dehydration, as well as vomiting and constant diarrhea, both including bleeding. Historians disagree about whether the epidemic was most likely measles, malaria, plague, smallpox, or perhaps typhus. In 2015, research by Powel Kazanjian at the University of Michigan suggested it could perhaps even have been Ebola, which could have jumped from fruit bats to humans. They are known to carry Ebola today and they have long been a food source in sub-Saharan Africa. Whatever it was seems to have killed about a quarter of the population.
Himself a survivor of the disease, Thucydides describes its symptoms and the course of the disease as it led towards death. He also describes how people reacted:
An aggravation of the existing calamity was the influx from the country into the city [for protection from the invading enemies], and this was especially felt by the new arrivals. As there were no houses to receive them, they had to be lodged at the hot season of the year in stifling cabins, where the mortality raged without restraint.
The bodies of dying men lay one upon another, and half-dead creatures reeled about the streets and gathered round all the fountains in their longing for water. The sacred places also in which they had quartered themselves were full of corpses of persons that had died there, just as they were; for as the disaster passed all bounds, men, not knowing what was to become of them, became utterly careless of everything, whether sacred or profane.
All the burial rites before in use were entirely upset, and they buried the bodies as best they could. Many from want of the proper appliances, through so many of their friends having died already, had recourse to the most shameless sepultures: sometimes getting the start of those who had raised a pile, they threw their own dead body upon the stranger's pyre and ignited it; sometimes they tossed the corpse which they were carrying on the top of another that was burning, and so went off. [Thucydides §52/p. 68]
Nor was this the only form of lawless extravagance which owed its origin to the plague. Men now coolly ventured on what they had formerly done in a corner … so they resolved to spend quickly and enjoy themselves, regarding their lives and riches as alike things of a day. Perseverance in what men called honour was popular with none, it was so uncertain whether they would be spared to attain the object. …
Fear of gods or law of man there was none to restrain them. As for the first, they judged it to be just the same whether they worshipped them or not, as they saw all alike perishing; and for the last, no one expected to live to be brought to trial for his offences, but each felt that a far severer sentence had already passed upon them all … . [Thucydides §53/p. 69]
The breakdown of law and order, the callousness toward the infected as being already the dangerous walking dead, and the fruitless appeals to religion are all reflected in this account of desperate people lacking the knowledge necessary to deal effectively with the tragedy that overcame their city. To hear Thucydides tell the story, it is hard to believe that anyone would ever again have faith in the Athenian gods, or in the legal system or codes of honor that in normal times defined an upstanding person. But an interestingly contrasting case of human response comes from China, and will serve as our third and last case study.
In the early 1940s, much of China was occupied by the Japanese, who were actively at war with China, as well as with the United States and other countries. Beginning in 1937, Japan had invaded and occupied large areas of China. A young man named Francis L. K. Hsu [Xǔ Lǎngguāng 许烺光, 1909-1999] had just received a Ph.D. degree in social anthropology from the London School of Economics and was newly appointed to National Yunnan University 国立云南大学 in Kūnmíng 昆明, in Yúnnán 云南 Province, an area of southwestern China that the Chinese government still controlled.
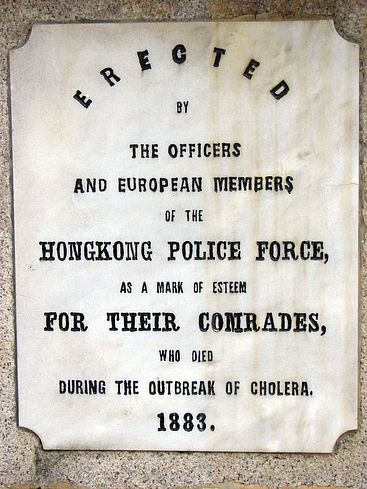
Despite the wartime conditions, young Dr. Hsu undertook a period of fieldwork from 1941 to 1943 in a remote village which he called by the pseudonym "West Town." In May and June of 1942, while Hsu was living in West Town, the village suffered a brief cholera epidemic, which killed many people. His observations and analysis of the epidemic, set against the background of war-time China, were recorded in a short book, published in 1952, Religion, Science, and Human Crises. The work is especially valuable because it is one of the very few accounts of an epidemic recorded by an ethnographically trained observer who lived through it during scheduled fieldwork.
Several competing responses to the epidemic are described, both religious and non-religious. As in most crises, many people were deeply skeptical of at least some of the views and approaches taken by their neighbors. But as deaths multiplied, so did the intensely felt need for solutions.
… Only a few deaths occurred at first; then heavier tolls were taken. For a period of time there were six or seven deaths per day even within the four gates of the town. There were many more in the outlying areas. The price of coffins rose from five hundred [Chinese] dollars each to two or three thousand dollars each. Later coffins were not to be had at any price. Carpenters, working day and night, made a tremendous profit out of the extraordinary demand.
Funeral processions became a common sight. At first these processions were simple or elaborate according to the means of the family of the dead. Later all processions became hasty and comparatively simple affairs. [Hsu, p. 10]
Note 10 The Chinese word tán 坛 is usually translated “altar,” but more often refers either to an open air platform for the conduct of public religious rites or to the enclosed chapel or tent where a Daoist priest performs rites.
Hsu tells us that the deaths began at about the beginning of the fourth Chinese lunar month, and the epidemic itself lasted only a little over a month in total. It took about a week for the people to notice that something was very wrong, and in response “prayer platforms” —apparently makeshift chapels— were constructed both within the town and in the surrounding countryside. [Note 10] These were sites where Daoist priests and representatives of the community conducted prayer sessions, sometimes lasting several days running. Hsu describes the goals of these sessions as three:
(1) supplication to gods who might either have ordered the epidemic as a measure of punishment against a sinning populace or have the power of driving it away; (2) coercion of gods who were believed directly to have produced the epidemic; and (3) comfort for, and elevation of, the dead. [Hsu, p. 14]
The influence of human morality on cosmic events is a very ancient tradition in China. (Excursus) Accordingly, a great deal of emphasis was put upon moral exhortations and upon various taboos or abstentions to be undertaken as signs of piety. For example, posters were put up prohibiting the sale of fish and meat, not out of a fear that fish and meat might bear disease, but because vegetarianism, according to Chinese Buddhist and folk tradition, is regarded as a good deed and a sign of a person’s religious merit. Other posters urged people to be kind, or to repent of their earlier sinful ways. A notice from the chief priest even listed all of the boorish acts he had noticed among attendees at these meetings, and condemned those who were not properly reverential, saying they were effectively inviting the epidemic onto themselves.
Some religious gatherings were devoted to the recitation of incantations or the chanting of Buddhist and Daoist scriptures. Other gatherings focused mainly on Daoist ritual, sending written petitions to the gods asking for their mercy and assistance.
The chief priest, followed by his assistants and musicians, in full ritual dress and regalia, would step down from the main platform. Holding a petition in one hand and a bell in the other, they would walk around the centre platform. As they did so he would ring his bell and the musicians would play, while all priests chanted passages from the scriptures in chorus. They would first walk slowly, but as time went on, their steps would gain momentum, and the music and the chanting would be louder. [Hsu, p. 17]
Then the priest would light the petition papers to transmit their contents to the gods. When all of the petitions had been burned, the ashes would be scattered over the little lake in the village.
At such gatherings some of the priests also wrote charms or amulets on sheets of paper, which were distributed free of charge through local dispensaries. The intention was to frighten away the cholera-bearing demons, or to capture them, depending upon the charm. These charms were posted over people’s doors for a day or for a longer period, and then the demon-capturing ones were burned at the center of the town “so that spirits which attempted to enter the families with intention of spreading the disease would be destroyed by them. (p. 20)”
For one of the multi-day rituals, Hsu tells us that
An effigy of the Wēn [瘟 epidemic] God was made as a part of the commencement of the prayer meeting which took place at the centre of the town. It was displayed prominently near the prayer platform. This effigy was impressive, about 15 feet tall, and very broad of body, dressed in glowing purple, gold and red. The features of his face were ferocious looking, such as bulging eyes, red whiskers and protruding incisors. It was supported by a heavy stick at the back, so that it could remain standing. [Hsu, p. 20]
On the fourth evening of this ritual, the figure was carried through the town, accompanying priests stabbing at the air with swords and dragging iron chains, while others shouted “U-woo” and “Open up,” imitating the sounds of plague demons seeking to enter houses. All of the people locked their doors tightly to avoid having any of the demons enter. At each household’s door the procession collected one of the demon-capturing charms. The charms were then loaded into a large boat made for the purpose and carried with the procession. Finally, with a great deal of additional chanting and prayer and the uttering of many charms, the boat was taken about a mile out of town and burned. [Note 11]
Note 11 The use of boats to dispose of epidemic demons is a very old and very widespread one in China, although often it is performed as a precaution when there is no active epidemic. See Katz 1995.
There were some Christian families in West Town, and they held their own prayer meetings, offered their own prayers, and produced their own amulets to be pasted up on houses.
At the same time that these measures were being taken by the established priests and the town’s leading citizens, various other actions were also being taken. People began concocting and selling medicines, advice, or proprietary methods of cure, often with extravagant promises and at high prices. Some, as an act of merit, offered their creations for free. Many people pasted additional charms on the walls of their houses, in addition to those passed out by the priests, and there was a great market in amulets promising protection.
Non-religious actions were taken as well, although sometimes they had connections to religious belief. Public health officials did offer injections of various antibiotics, and a few people got them. The village water came from streams flowing to a nearby lake. West Town was one of the last villages through which the streams flowed, and most water was already dirty when West Towners washed their clothes and vegetables in it or added their sewage to it. When the epidemic became evident, many people stopped using these streams. Public health officials were happy about this. People’s reasons, however, were not exactly just a matter of human health. Hsu writes:
When asked about the reason for this measure [avoiding stream water] the answer was that it was to clean up the area for the gods, because washing clothes and food in these streams caused the pollution of the water, which ran down from the mountains (where the God of Mountains resides) to the lake (where the Dragon God and his family reside). [Hsu, p. 46]
For the same reason —to clean things up to please the gods— people swept streets, avoided spitting in public as much as usual, and straightened and cleaned their compounds.
Many people reexamined their diets:
… the entire community almost automatically imposed on itself a taboo on many varieties of food. Food which was normally served in the streets and eaten cold, like pea-curd and bean-custard (not bean-curd), were not eaten at all because the local people said ‘they make the abdomen cold’. For the same reason, any vegetable or fruit which was customarily regarded as ‘cold-producing’ was also tabooed. The list of tabooed foods was as follows: potato (the price of which dropped all of a sudden from three dollars to fifty cents a catty), string beans, turnip, all sour fruit (plums in particular, because they were in season), confections, new wheat flour, fresh meat, fish (the pious would not touch any meat or fish, even preserved, others were less stringent in their observances), pumpkin, egg plant, etc. It will be noted that this list included practically all fresh fruit and vegetables from the field except cabbage, garlic, pepper and a few others. (The word “cold” here used has little to do with the temperature as in the West. It refers to an inner coldness which is only defined traditionally. …) [Hsu p. 45]
Some of the measures directed at spirits corresponded with actions that might have been recommended by public health workers around the world, for they involved avoiding contaminated water —the main way in which cholera is spread— and generally cleaning up sources of contamination, but it is important to note that the motivations were not necessarily related to anything known about cholera so much as about gods and demons.
It had been hot and dry for most of the month. Hsu tells us that a few days before the last large-scale religious ritual, rain began to fall, driving the temperature down significantly. Cholera, as we noted earlier, has an optimum temperature of about 27°C, and does not survive well below 15°. Thus with the last major ritual the epidemic ended.
Hsu was impressed that the ending of the epidemic was understood to be evidence of the efficacy of the many and various ways of dealing with the crisis: the food taboos, the prayers, the charms, the burning boat. None of his informants said anything about the temperature, and few thought the inoculations made any more difference than the religious activities.
Although an archaeological body count may suggest prehistoric catastrophe, it tells us little about the human understanding of what was happening. Each of these three examples —the decimation of the Upper Missouri tribes, Thucydides describing the widespread breakdown and panic in Athens, and Hsu describing methodical but unscientific responses to a brief cholera epidemic in war-time Yunnan— has its own lessons to teach. It is inviting to speculate on what would have happened to relations among the Greek cities if their epidemic had been as all-devouring as the one that overcame the Hidatsa and Mandan, or to ask whether Chinese religion could have remained credible if the cholera epidemic in Yunnan had lasted as long as the one in Athens.
But these cases at the very least remind us that people are not merely passive victims of the diseases to which we are heir. On the contrary, diseases are part of the total environment to which we humans adjust our lives, and to which we bring all our wit, philosophy, charity, greed, insight, fear, and opportunism. Humanity is still here. Sadly, so are the cholera demons. And the Copts have lost their pigs. But at least we have conquered smallpox.
Four review quizzes are available for this reading: Quiz 1, Quiz 2, Quiz 3, Quiz 4.
On this web site, additional notes are available for the following diseases:
AIDS,
anthrax,
cholera,
dengue fever,
influenza,
malaria,
plague,
smallpox,
measles,
thyphoid,
tuberculosis,
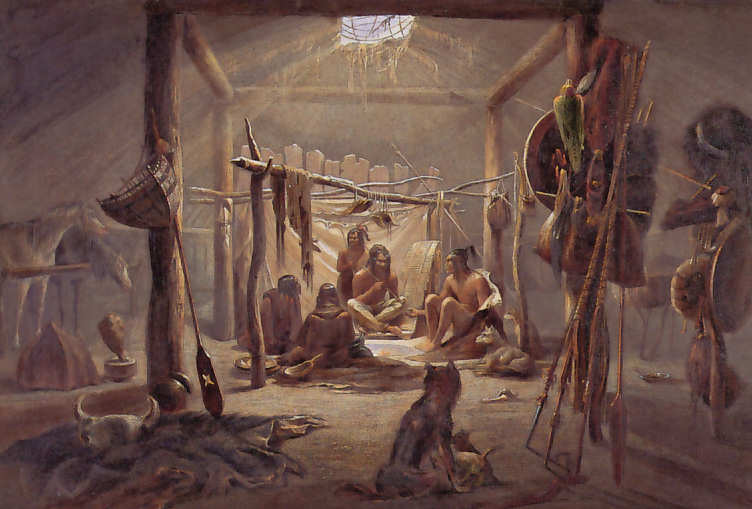
Further note: Two pictures by Karl Bodmer, “Mató Tópe Killing a Cheyenne Chief” (Joslyn Art Museum, Omaha) and “A Mandan Chief’s House” (Library of Congress), were apparently first published in black and white in Germany as part of Prince Maximilian of Wied's North American travel journals in 1839-41, where they were plates 19 (Mandan) and 22 (killing). The color versions apparently were published in 1834 and have been reproduced in a range of works ever since.